Sham acupuncture in chronic pain – The BMAS Blog

Inspired by Zhou et al 2022.[1]
MA – meta-analysis
NMA – network meta-analysis
IPDM – individual patient data meta-analysis
RA – real acupuncture
SA – sham acupuncture
NPSA – non-penetrative SA
PSA – penetrative SA
NA – no acupuncture
RCT – randomised controlled trial
HRQoL – health-related quality of life
ANCOVA – analysis of covariance
ES – effect size
EA – electroacupuncture
TENS – transcutaneous electrical nerve stimulation
AE – adverse eventkey to acronyms
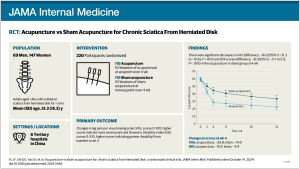
This is a network meta-analysis (NMA) of acupuncture in chronic pain from Guangzhou that specifically aimed to assess the relative merits of different forms of sham acupuncture (SA).
It is the first NMA to compare different forms of SA, but not the first NMA to include SA.[2] It is also not this first time penetrative and non-penetrative shams have been assessed,[3] although it is the first time this has been done in an NMA.
This NMA includes 62 RCTs and a total of 6806 patients and finds no statistically significant differences between NPSA, PSA and NA. The IPDM update by Vickers et al (2018) included 39 trials and 20 827 patients.[3] It found a significant difference in the size of the effect when RA was compared with NPSA as opposed to PSA. You might think that the IPDM was simply more powerful; however, it only included 21 sham controlled RCTs with 6276 patients.
Saramago et al used the data from the original version of the IPDM (2012) [4] to perform the first NMA of continuous outcomes.[2] They showed significant differences between SA and NA for HRQoL outcomes, but not for pain outcomes.
Why the differences? Much probably derives from the inherent power of the IPDM process, where the individual data is reanalysed using ANCOVA. This does not change the results in terms of mean differences, but it can provide greater statistical power where there are baseline differences and poor correlation between baseline and end scores.[5]
The other key difference is the fact that most of the huge German ARC and GERAC trials are included in the IPDM but not in this NMA.
But it uses only one third of the available data…
Why should we be bothered by this result? Zhou et al conclude that SA has a weak but non-significant effect and therefore can be used as an inert placebo control in acupuncture RCTs. But it uses only one third of the available data, and importantly excludes all of the huge RCTs from Germany with comparisons of SA with NA. In these NA was often guideline-based conventional care.
You only have to consider the results of Haake et al,[6] where SA was 50% better than guideline-based conventional care in chronic low back pain, to have considerable doubts about the validity of Zhou et al’s conclusion, at least for research conducted in the West.
SA was 50% better than conventional care in chronic low back pain
Haake et al 2007 [6]
Having said that, there does seem to be a difference appearing between the effect sizes of shams in the East and the West. There are all sorts of factors that could influence these differences of course, not least of which are the comparators, populations and the degree to which bias can be excluded.
Going back to the Vickers et al IPDM,[3] the difference in ES for RA versus NPSA and RA versus PSA only narrowly reached significance, and was not significant when outlying trials were excluded.[7–9] These outlying trials used strong EA versus NPSA (sham EA) and strong RA versus sham TENS, so they were maximising the physiological differences between stimulation strength.
It is possible that the strength and intensity of RA used in RCTs in the East is consistently greater than that in the West. This would be consistent with the idea that we need to be more careful with our choice of SA in the West than our colleagues do in East.
It is possible that RA is stronger and more intense in the East than in the West…
On an entirely different matter, in view of the unexpected mention of an acupuncture AE in the football news, I will just highlight another case of haemothorax following acupuncture.[10] This time it was from Korea and the case report published in Acupuncture in Medicine has some great thoracoscopic images, which allow a convincing degree of understanding of the mechanism.
References
1 Zhou R, Zhu Y-J, Chen X, et al. Effect of Sham Acupuncture on Chronic Pain: A Bayesian Network Meta-analysis. Pain Med Published Online First: 22 August 2022. doi:10.1093/pm/pnac126
2 Saramago P, Woods B, Weatherly H, et al. Methods for network meta-analysis of continuous outcomes using individual patient data: a case study in acupuncture for chronic pain. BMC Med Res Methodol 2016;16:131. doi:10.1186/s12874-016-0224-1
3 Vickers AJ, Vertosick EA, Lewith G, et al. Acupuncture for Chronic Pain: Update of an Individual Patient Data Meta-Analysis. J Pain 2018;19:455–74. doi:10.1016/j.jpain.2017.11.005
4 Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med 2012;172:1444–53. doi:10.1001/archinternmed.2012.3654
5 Vickers AJ, Altman DG. Statistics notes: Analysing controlled trials with baseline and follow up measurements. BMJ 2001;323:1123–4. doi:10.1136/bmj.323.7321.1123
6 Haake M, Müller H-H, Schade-Brittinger C, et al. German Acupuncture Trials (GERAC) for chronic low back pain: randomized, multicenter, blinded, parallel-group trial with 3 groups. Arch Intern Med 2007;167:1892–8. doi:10.1001/archinte.167.17.1892
7 Vas J, Méndez C, Perea-Milla E, et al. Acupuncture as a complementary therapy to the pharmacological treatment of osteoarthritis of the knee: randomised controlled trial. BMJ 2004;329:1216. doi:10.1136/bmj.38238.601447.3A
8 Vas J, Perea-Milla E, Méndez C, et al. Efficacy and safety of acupuncture for chronic uncomplicated neck pain: a randomised controlled study. Pain 2006;126:245–55. doi:10.1016/j.pain.2006.07.002
9 Vas J, Ortega C, Olmo V, et al. Single-point acupuncture and physiotherapy for the treatment of painful shoulder: a multicentre randomized controlled trial. Rheumatology 2008;47:887–93. doi:10.1093/rheumatology/ken040
10 Lee SS. Acupuncture-induced hemopneumothorax: a case report. Acupunct Med Published Online First: 19 August 2022. doi:10.1177/09645284221117843