Where to needle 2022 – The BMAS Blog
…in two tricky muscles!
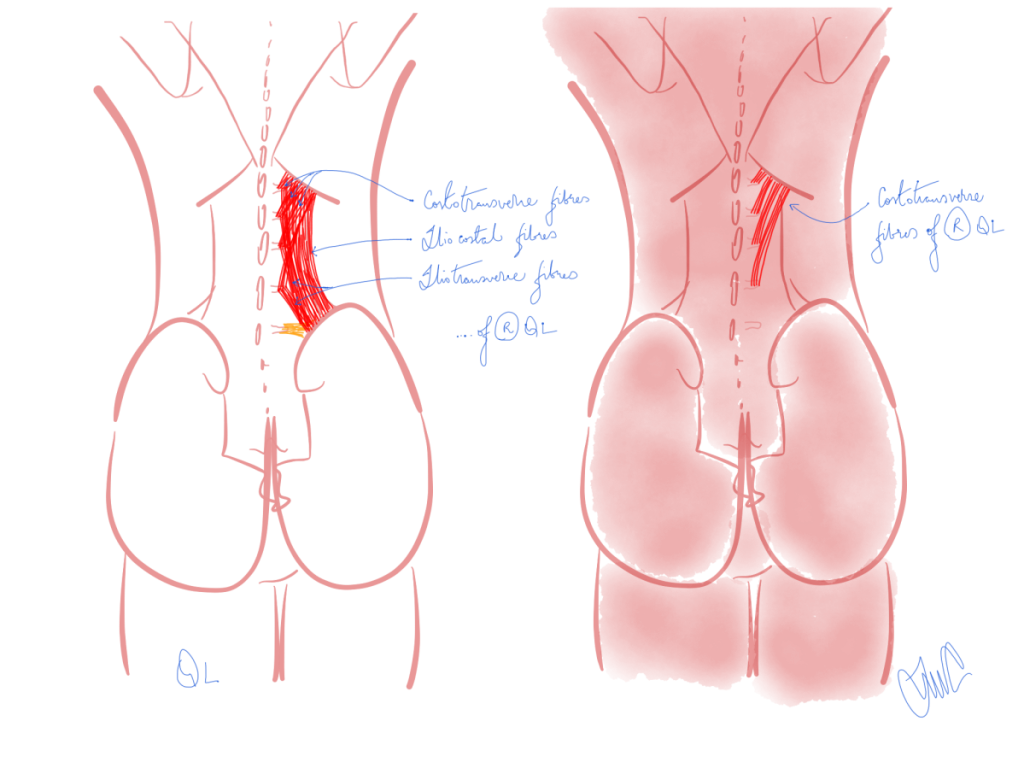
Inspired by Yi et al & Lee et al 2022.[1,2]
-
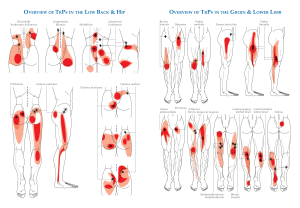
Drawing by MC to illustrate the 3 different sets of fibres making up QL (left) and the just the costotransverse fibres (right). -

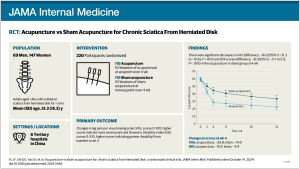
Screenshot from the BMAS Points Resource (QL) with QL fibres and their attachments drawn in over the image.
SR – systematic review
QL – quadratus lumborum
EPZs – endplate zones
TrPs – trigger points
SS – supraspinatus
TPs – transverse processeskey to acronyms
Enough of SRs and meta-regression, this week we take a dive into muscle innervation as a means of determining the best zone to needle in a couple of tricky muscles.
Both papers come from the same group in South Korea and utilise the same method for visualising neural innervation of cadaveric muscle – the modified Sihler’s staining method. This method is a multistep process that takes over 3 months and eventually allows visualisation of neural arborisation within the muscle.
the modified Sihler’s staining method
In the first of these two studies,[1] 15 quadratus lumborum (QL) muscles from 5 male and 5 female cadavers were dissected out before being subjected to the staining method. The areas of neural arborisation were noted based on the position of bony anatomical landmarks. The presence of increased neural branching is in the same area as the endplate zones (EPZs) of the muscle, and therefore may indicate the best areas to target for certain therapeutic approaches. The authors here are interested in finding the best areas for injection of botulinum toxin; however, the same areas are likely to be harbouring TrPs, so may be useful for us as acupuncturists and dry needling enthusiasts.
In QL the key areas were between L3 and L4 in the middle and lateral aspects of the muscle and below L4 in the middle aspect of the muscle.
The second paper does the same thing for the supraspinatus (SS) muscle.[2] Seventeen SS muscles were dissected from 15 embalmed cadavers – 8 male and 7 female specimens. The muscle was stained and divided for the purposes of reporting the results into 4 equal portions (A to D) from medial to lateral. Each section was roughly 2 finger breadths wide. Nerve entry points were in B and C but not in A or D. These positions probably correlate best to SI12 and LI16.
Whilst QL is commonly tender, TrP bands are rarely easy to palpate, so knowing the areas most likely to harbour EPZs and therefore TrPs is quite useful. SS is not as deep as QL, but is covered by trapezius, so bands are also difficult to palpate in this muscle.
Clinically we are guided by tenderness and pain recognition on palpation. I find this useful in QL but not so much in SS, where there is much potential for confounding due to trapezius overlying the bony edges of the scapula. I have often been convinced of finding TrPs in the upper section of QL just beneath the 12th rib. That area did not figure in this anatomical study by Li et al,[2] but one of their figures does show a branch of the iliohypogastric nerve entering high on the medial aspect of the muscle. I imagine it is likely that the costotransverse slivers of QL from the TPs of L1, L2, and L3 to the 12th rib could have EPZs and hence TrPs relatively high in the muscle.
It is interesting to note that both QL and SS have 3 parts. Arguable, QL is the more complex structurally due to all the slivers of muscle to and from the lumbar TPs, but the structural organisation of most muscles is much more complex than we often appreciate. For example, SS is a pennate muscle with 3 heads that insert into a tendon that stretches almost half the length of the muscle.
the structural organisation of most muscles is much more complex than we often appreciate
Since these papers are principally concerned with sites for injection, I should note that injections of botulinum toxin or indeed any other substance have not been demonstrated to work better than saline injection in myofascial pain,[3,4] but short term benefits of wet needling TrPs with local anaesthetic in neck pain have been demonstrated over dry needling with low certainty.[5] As we learned in the blog last week (), the effect size for acupuncture in myofascial pain has been measured as large with moderate certainty.[6]
References
1 Yi K-H, Lee K-L, Lee J-H, et al. Guidance to trigger point injection for treating myofascial pain syndrome: Intramuscular neural distribution of the quadratus lumborum. Clin Anat Published Online First: 2 June 2022. doi:10.1002/ca.23918
2 Lee H-J, Lee J-H, Yi K-H, et al. Intramuscular Innervation of the Supraspinatus Muscle Assessed Using Sihler’s Staining: Potential Application in Myofascial Pain Syndrome. Toxins 2022;14:310. doi:10.3390/toxins14050310
3 Cummings TM, White AR. Needling therapies in the management of myofascial trigger point pain: A systematic review. Arch Phys Med Rehabil 2001;82:986–92. doi:10.1053/apmr.2001.24023
4 Soares A, Andriolo RB, Atallah AN, et al. Botulinum toxin for myofascial pain syndromes in adults. Cochrane Database Syst Rev 2014;:CD007533. doi:10.1002/14651858.CD007533.pub3
5 Navarro-Santana MJ, Sanchez-Infante J, Gómez-Chiguano GF, et al. Dry Needling versus Trigger Point Injection for Neck Pain Symptoms Associated with Myofascial Trigger Points: A Systematic Review and Meta-analysis. Pain Med Published Online First: 11 June 2021. doi:10.1093/pm/pnab188
6 Yuan Q-L, Wang P, Liu L, et al. Acupuncture for musculoskeletal pain: A meta-analysis and meta-regression of sham-controlled randomized clinical trials. Sci Rep 2016;6:30675. doi:10.1038/srep30675
Published