Acupuncture for chronic sciatic 2024 – The BMAS Blog

Inspired by Tu et al 2024.[1]
IF – impact factor
BUCM – Beijing University of Chinese Medicine
RCT – randomised controlled trial
VAS – visual analogue score
ODI – Oswestry Disability Index
MCID – minimum important clinical difference– key to acronyms
A general internal medicine physician colleague from UCLH picked up this paper from JAMA Internal Medicine (IF 39.0) just before it appeared in my searches. I met the first author and the last author at a recent acupuncture conference in Jeju, South Korea. Neither of them mentioned that this paper was due out, but then again, neither of them spoke fluent enough English for more than a greeting and a nod (similarly my Mandarin did not allow for much beyond ???). Their younger female colleagues were much more animated and communicative and less linguistically challenged than us chaps (no surprises there). They were quick to organise a photo and invite me to BUCM, which was nice. I told them I had already visited, but probably before their time.
BUCM, where Tu Jianfeng (first author) and Liu Cunzhi (last author) are based, was the venue for my first conference presentation in China, back in 2012. It was the 30th anniversary of the School of Acupuncture–Moxibustion and Tuina at BUCM and the 3rd International Symposium of Techniques of Acupuncture–Moxibustion and Tuina. Incidentally, the dean of BUCM at the time was Prof Zhao Baixiao and I met him again recently in London at WFAS 2024.

This image is care of Zhou Hang (thank you) who is on the far right.
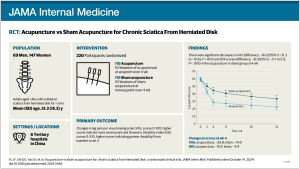
This is a moderately (n=220) large multicentre sham controlled RCT with 2 parallel arms carried out at 6 hospitals in China. The patient population were adults with unilateral sciatica from a herniated lumbar disc for at least 3 months. Their leg pain had to score 40 or more on VAS.
Acupuncture or sham acupuncture was applied in 10 sessions over 4 weeks and the follow-up extended to 52 weeks. Outcomes were recorded at several time points, but the primary outcomes (change in VAS leg pain and the ODI) were measured between baseline and 4 weeks (ie immediately after the treatment period).
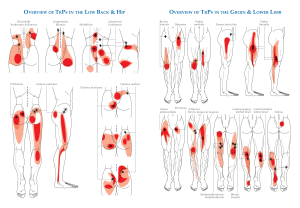
The acupuncture treatment involved bilateral points in the back (BL25 BL26) and unilateral points in the leg depending on the site of the leg pain (GB30, 31, 33, 34, 39 or BL54, 36, 40, 57, 60). If the patient had pain at the back of the leg and at the side of the leg, the practitioner could choose any 5 points from those listed. Hwato needles of 0.30mm diameter and 40mm to 75mm were used. The longer needles were used at GB30 and BL36, and at the back points. Needles were inserted 40mm to 50mm at the former points and 30mm to 40mm at the back points.
So, in total I calculate 9 points were used in each patient at each session and there were 3 sessions a week for the first 2 weeks followed by 2 sessions a week until the 4-week point.
The sham was performed at non-points adjacent to the points listed for the real acupuncture using shorter blunt needles and adhesive foam discs of 10mm diameter and 5mm depth. The same adhesive discs were used in the real acupuncture group, so I wonder to what degree this may have inhibited the ability to manipulate the needles (I’ll ask). At one point in the sham group a real needle was inserted in an attempt to improve blinding. It was inserted 25mm to 40mm in a non-point lateral to BL37 in the mid posterolateral thigh and was not manipulated.
Blinding was successful and apparently the adhesive pads did not inhibit needle manipulation too much (thanks to Zhou Hang from BUCM for the extra information via WeChat). The adhesive foam pads were relatively loose foam so that they held the blunt needles ok but only minimally restricted the manipulation of the real needles.
The patients were aged just over 50 (mean) and there were twice as many women as men. The mean baseline VAS leg pain was 60 and ODI (0 to 100) was 34.
At 4 weeks the mean VAS leg pain was 29 in the acupuncture group and 45 in the sham group and ODI was 21 and 30 respectively. The MCIDs for these measures was taken to be 15mm on the VAS and 7 points on the ODI. Both were just achieved in terms of between group differences although I have argued many times that mean group differences have no relevance to individual patients who only care about their own change from baseline values.
The change from baseline in the acupuncture group at 4 weeks was 31 on VAS leg pain and 11 on the ODI. In the sham group these changes were 15 and 7 (rounded up from 14.5 and 6.7).
So, this is a very well designed and conducted piece of research and the treatment protocol is just achievable in the West, with a bit of increased capacity. I realised some years ago that initial treatment of acute sciatica with acupuncture needed sessions at least twice a week and ideally 3 times, as they did in this study. Together with the previous data on inflammation preserving treatment (see: )[2] this research adds a strong indication that the best treatment for acute sciatica is likely to be a combination of acupuncture and the avoidance of NSAIDs or steroids, so that adequate pain relief is combined with more rapid resorption of the rogue extruded disc material.
References
1 Tu J-F, Shi G-X, Yan S-Y, et al. Acupuncture vs Sham Acupuncture for Chronic Sciatica From Herniated Disk: A Randomized Clinical Trial. JAMA Intern Med. Published Online First: 14 October 2024. doi: 10.1001/jamainternmed.2024.5463
2 Albert HB, Sayari AJ, Barajas JN, et al. The impact of novel inflammation-preserving treatment towards lumbar disc herniation resorption in symptomatic patients: a prospective, multi-imaging and clinical outcomes study. Eur Spine J. 2024;33:964–73. doi: 10.1007/s00586-023-08064-x
Published