Acupuncture for DLSS – The BMAS Blog
Stimulated by Zhu et al 2024.[1]
DLSS – degenerative lumbar spinal stenosis
IF – impact factor
RCT – randomised controlled trial
NRS – numerical rating scale
RMDQ – Roland Morris disability questionnaire
MCID – minimum clinical important difference
SSSQ – Swiss spinal stenosis questionnaire– key to acronyms
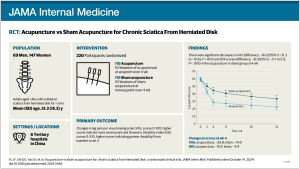
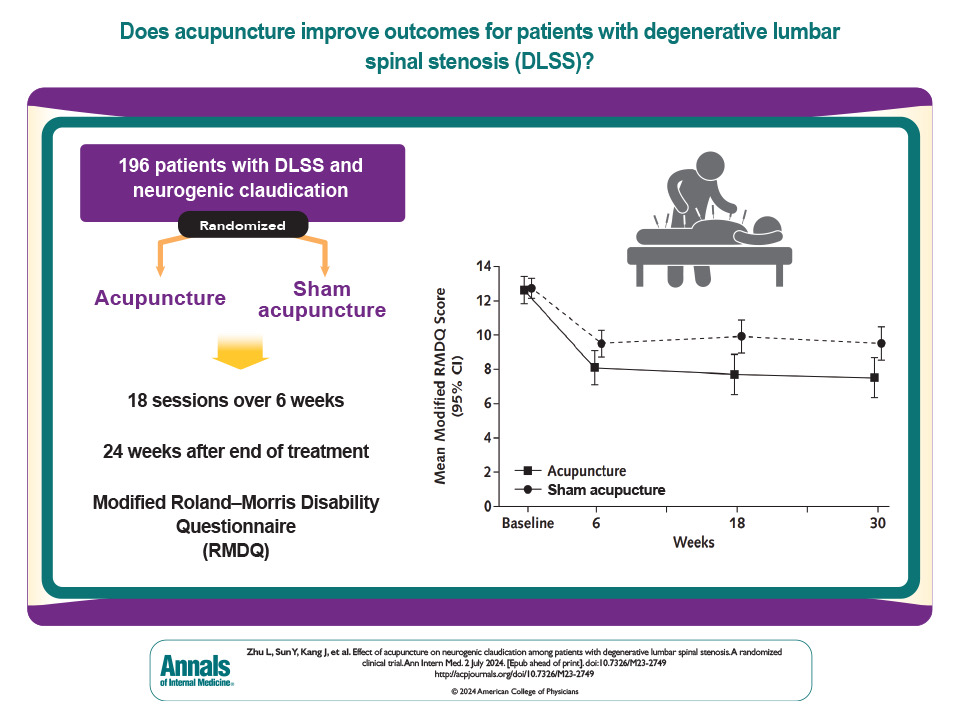
This paper in Annals of Internal Medicine (IF 39.2) reports on a multi-centre sham controlled RCT (n=196) from 5 hospitals in China. The paper comes from a well-known group based at the China Academy of Chinese Medical Sciences in Beijing.
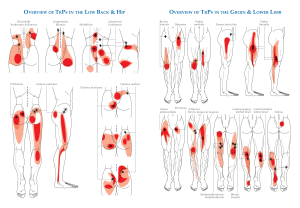
As suggested by the full title of the paper, which refers to neurogenic claudication, the primary outcome was leg pain rather than back pain. The population was selected from patients who were 50 to 80 years old with neurogenic claudication (buttock and or leg pain) attributed to central DLSS. The buttock or leg pain had to be more severe than the back pain and at least 4 out of 10 on NRS. They also had to score at least 7 on the RMDQ (a 24-item scale).[2]
This must be the largest trial to date for this indication (published in English) and a recent review on neurogenic claudication by Ammendolia et al [3] only found 2 acupuncture trials.[4,5] One of the latter came from the same group as the current trial. It was essentially the pilot study (n=80) for this larger RCT, but whilst the acupuncture intervention was the same, the sham control was changed from a non-penetrating to a penetrating sham.
Acupuncture treatment was performed 3 times a week for 6 weeks, making a total of 18 sessions. The protocol include 5 bilateral points: BL23, BL25, BL40, BL57, KI3. The one thing that made this protocol slightly different was that at BL25 the needles were inserted 50 to 70mm until the patient experienced an electric shock sensation to the knees and posterior lower legs, at which point, the needles were lifted 1 to 2mm. Standard needling depths were used at the other points. So, at BL25, the intention was to get very close to the L4 spinal nerve.
The sham technique was a little unusual as well. Whereas, in the pilot study, non-penetrating needling was used at the same points, in this trial they swapped to superficial needling with no sham device, but it was still performed at the same ‘real’ acupuncture points.
The primary outcome was the change from baseline in the RMDQ at 6 weeks. The MCID for the RMDQ has been estimated to be 2-3 points.[6]
In the acupuncture group the RMDQ fell from a baseline of 12.6 to 8.1 at 6 weeks. In the sham (superficial on-point needling) group the RMDQ fell from a baseline of 12.7 to 9.5 at 6 weeks. So, there was a clinically important change from baseline in the sham group. There was a larger fall in the acupuncture group with deep needling. The adjusted difference in mean change of the RMDQ was 2.1 (p=0.044), just reaching statistical significance, but perhaps questionable in terms of clinical significance to some eyes. Of course, the difference here is between two different needling styles applied to the same acupuncture points.
The authors point out that their results compare favourably to the only effective non-surgical intervention for neurogenic claudication – a multimodal approach including manual therapy and exercise. They quote a figure of 20% of patients achieving a minimal clinically meaningful improvement (a 30% reduction in SSSQ) after 8 weeks of manual therapy and individualised exercise. The equivalent figure for the same outcome measure in this trial was 55.4%.
References
1 Zhu L, Sun Y, Kang J, et al. Effect of Acupuncture on Neurogenic Claudication Among Patients With Degenerative Lumbar Spinal Stenosis: A Randomized Clinical Trial. Ann Intern Med. Published Online First: 2 July 2024. doi: 10.7326/M23-2749
2 Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8:141–4. doi: 10.1097/00007632-198303000-00004
3 Ammendolia C, Hofkirchner C, Plener J, et al. Non-operative treatment for lumbar spinal stenosis with neurogenic claudication: an updated systematic review. BMJ Open. 2022;12:e057724. doi: 10.1136/bmjopen-2021-057724
4 Kim KH, Kim YR, Baik SK, et al. Acupuncture for patients with lumbar spinal stenosis: a randomised pilot trial. Acupunct Med. 2016;34:267–74. doi: 10.1136/acupmed-2015-010962
5 Qin Z, Ding Y, Xu C, et al. Acupuncture vs Noninsertive Sham Acupuncture in Aging Patients with Degenerative Lumbar Spinal Stenosis: A Randomized Controlled Trial. Am J Med. 2020;133:500-507.e20. doi: 10.1016/j.amjmed.2019.08.038
6 Patrick DL, Deyo RA, Atlas SJ, et al. Assessing health-related quality of life in patients with sciatica. Spine. 1995;20:1899–908; discussion 1909. doi: 10.1097/00007632-199509000-00011
Published