Chronic primary MSK pain 2022 – The BMAS Blog

Inspired by a perspective and commentaries in Pain Reports.[1–3]
MSK – musculoskeletal
MPS – myofascial pain syndrome
WA – Western Australiakey to acronyms
A couple of these papers popped up on my searches on Friday 19th August, and since transport disruption had led to a cancelled clinic, I found myself being sucked into the traps, pitfalls, and murky waters of the commentaries.
I guess the first thing to say is that the chronic pain literature is dominated by clinicians and researchers who specialise in chronic pain rather than in MSK conditions. So, if the title of this blog attracted you because of the MSK included in it, you will probably be disappointed. There is no mention of any specific MSK conditions or how to treat them in these papers. They are essentially arguments over classification, nomenclature, and taxonomy. But myofascial pain is mentioned, hence the papers came up on my searches, and it is interesting to review the debate.
The perspective paper by Fitzcharles et al was stimulated by the release of ICD-11 in February 2022,[4] which includes the category chronic primary MSK pain (MG30.02)[5] under chronic primary pain (MG30.00),[6] which in turn is under chronic pain (MG30).[7] The latter chronic pain category also includes chronic secondary MSK pain.[8]
Below are the descriptions from ICD-11:
Chronic primary musculoskeletal pain is chronic pain in the muscles, bones, joints or tendons that is characterised by significant emotional distress (anxiety, anger/frustration or depressed mood) or functional disability (interference in daily life activities and reduced participation in social roles). Chronic primary musculoskeletal pain is multifactorial: biological, psychological, and social factors contribute to the pain syndrome. The diagnosis is appropriate independently of identified biological or psychological contributors unless another diagnosis would better account for the presenting symptoms. Other chronic musculoskeletal pain diagnoses to be considered are those listed under chronic secondary musculoskeletal pain.
Chronic secondary musculoskeletal pain is chronic pain arising from bone(s), joint(s), muscle(s), vertebral column, tendon(s) or related soft tissue(s). It is a heterogeneous group of chronic pain conditions originating in persistent nociception in joint, bone, muscle, vertebral column, tendons, and related soft tissues, with local and systemic aetiologies, but also related to deep somatic lesions. The pain may be spontaneous or movement-induced.
Fitzcharles et al propose a set of clinical characteristics to distinguish between primary and secondary MSK pain. They label secondary MSK pain as being predominantly nociceptive and primary MSK pain as being predominantly nociplastic. They note that secondary musculoskeletal pain includes conditions such as myofascial pain syndromes (MPS), arthritis and tendonitis; however, the latter two examples can be classified elsewhere in ICD-11, and it is only myofascial pain that is controversial here. Myalgia is tucked away elsewhere under miscellaneous specified soft tissue disorders,[9] but it is not clear to me that MPS should go there.
They also refer to chronic primary MSK pain as being best understood as ‘regional fibromyalgia’, which gets them roundly criticised by the commentators, but I know what they mean, and there is probably a lot of overlap mechanistically, should you ever actually find a patient with it, ie one who does not have any obvious sign of peripheral nociception.
The first of the commentators (Cohen ML) engages in a blistering attack that includes taxonomic, clinical, and mechanistic aspects.[2] Whilst technically correct, his taxonomic niggles are rather pedantic, although having similar tendencies myself I can hardly complain about technical precision. Cohen dismisses the mention of MPS out of hand, and it is only then that I realised this author has teamed up in the past with Quintner to deny the existence of MPS. Both from Perth, WA, they appear to be quite an argumentative pair who currently have , several of which are critical letters aimed at MPS or pain taxonomy.
Rolf-Detlef Treede, from the Department of Neurophysiology at Heidelberg University, is more supportive and positive in his commentary. He argues for a third column for MPS alongside primary and secondary MSK pain, although he too is not happy with the term ‘regional fibromyalgia’.[3] His reason for a third column is based on the uncertainty as to whether MPS represents a principally nociceptive or nociplastic phenomenon. When I am teaching, I use the terms peripheral and central components of pain to represent nociceptive and nociplastic aspects of a patient’s presentation since there is undoubtedly both of these involved in any single case.
The term nociplastic pain was proposed relatively recently.[10]
Pain that arises from altered nociception despite no clear evidence of actual or threatened tissue damage causing the activation of peripheral nociceptors or evidence for disease or lesion of the somatosensory system causing the pain.
Note: Patients can have a combination of nociceptive and nociplastic pain.
[11]
Interestingly, Cohen was involved in the process of proposing nociplastic pain,[10] and even argued with the critics,[12,13] but then he clearly fell out with the group and criticised their attempt to define clinical criteria.[14,15]
Having watched of the recent Pain paper on nociplastic pain I realised that I had met the lead author at dinner before speaking at a pain conference in Oslo (January 2020). Had I known she was leading the drive to define nociplastic pain, I would have had rather more to say.
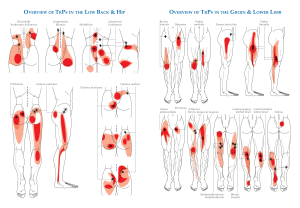
The bottom line for me is that I cannot recall any patient case for which I would have wanted to reach for the nociplastic label. This may be because I examine the MSK system of my patients thoroughly, know my anatomy well, and use fine filiform extensions of my examining fingers to probe deep somatic tissues and ask, “Is that your pain?” “Or is it a different pain in the same place?”
The point I am making is that if you have a good knowledge of the MSK system (the working parts – if bodies were machines) you can nearly always find a peripheral source of acute or chronic pain. The degree to which there are central components varies in individuals based on their genetic and environmental history, but to define a category of pain that is chronic, regional, and has no discernible peripheral nociceptive source strikes me as an excuse to continue failing to examine your patients thoroughly enough.
Harsh perhaps, but we do have a set of specialists who can train without needing to know either the names or the (pennate) structure of our major working parts, or knowing how to examine them. I have often heard such colleagues dismiss tender points, and therefore also trigger points, as a mere reflection of central processing, but even the great Patrick Wall was not able to respond (apart from with a smile) to my contention that it was physiologically impossible for an entirely central process to generate a discreet point of tenderness the size of an examiner’s fingertip. The smallest area I estimate would be around 5cm in diameter – the distribution of a single peripheral nociceptive neurone. In muscle tissue this would be at least the size of a golf ball, and probably considerably bigger.
References
1 Fitzcharles M-A, Cohen SP, Clauw DJ, et al. Chronic primary musculoskeletal pain: a new concept of nonstructural regional pain. Pain Rep 2022;7:e1024. doi:10.1097/PR9.0000000000001024
2 Cohen ML. Clarifying “chronic primary musculoskeletal pain”? The waters remain murky. Pain Rep 2022;7:e1021. doi:10.1097/PR9.0000000000001021
3 Treede R-D. Chronic musculoskeletal pain: traps and pitfalls in classification and management of a major global disease burden. Pain Rep 2022;7:e1023. doi:10.1097/PR9.0000000000001023
4 ICD-11 for Mortality and Morbidity Statistics. (accessed 20 Aug 2022).
5 ICD-11 MG30.02 Chronic primary musculoskeletal pain. (accessed 20 Aug 2022).
6 ICD-11 MG30.0 Chronic primary pain. (accessed 20 Aug 2022).
7 ICD-11 MG30 Chronic pain. (accessed 20 Aug 2022).
8 ICD-11 MG30.3 Chronic secondary musculoskeletal pain. (accessed 20 Aug 2022).
9 ICD-11 FB56.2 Myalgia. (accessed 20 Aug 2022).
10 Kosek E, Cohen M, Baron R, et al. Do we need a third mechanistic descriptor for chronic pain states? Pain 2016;157:1382–6. doi:10.1097/j.pain.0000000000000507
11 Terminology | International Association for the Study of Pain. Int. Assoc. Study Pain IASP. (accessed 21 Aug 2022).
12 Brummett C, Clauw D, Harris R, et al. We agree with the need for a new term but disagree with the proposed terms. Pain 2016;157:2876. doi:10.1097/j.pain.0000000000000717
13 Cohen M, Kosek E, Baron R, et al. Reply. Pain 2016;157:2876–7. doi:10.1097/j.pain.0000000000000718
14 Kosek E, Clauw D, Nijs J, et al. Chronic nociplastic pain affecting the musculoskeletal system: clinical criteria and grading system. Pain 2021;162:2629–34. doi:10.1097/j.pain.0000000000002324
15 Cohen ML. Proposed clinical criteria for nociplastic pain in the musculoskeletal system are flawed. Pain 2022;163:e606–7. doi:10.1097/j.pain.0000000000002505