MSK mimics of LS radiculopathy – part 2 – The BMAS Blog
Stimulated by Jorgensen et al 2024.[1]
MSK – musculoskeletal
LS – lumbosacral
IF – impact factor
EDX – electrodiagnostic medicine
NCS – nerve conduction studies
MPS – myofascial pain syndrome
FAI – femoroacetabular impingement
TrPs – trigger points (myofascial is implied)
GTPS – greater trochanteric pain syndrome
US – ultrasound
GT – greater trochanter
ITB – iliotibial band
SIJ – sacroiliac joint
IMHO – in my humble opinion– key to acronyms
This is part 2 of a topic I covered on the blog in May this year – see: . It is published in the journal Muscle Nerve (IF 3.4), and principally aimed at EDX specialists.
Part 2 covers the most common sources of pain that mimic LS radiculopathy. 11 sections of the paper cover 9 condition labels and an introduction and conclusion. There are only 26 references in this paper compared with 174 in part 1.[2]
The aim of the article seems to be to give EDX specialists a shortlist of conditions to consider when their primary diagnostic tests (eg NCS) are negative in patients referred for assessment of LS radiculopathy. The article also suggests some simple MSK tests to help the choice of MSK label.
The first listed MSK mimic for LS radiculopathy is facet joint arthropathy. The main source of information (and only reference in this section) comes from a paper I have mentioned previously on the blog webinar (29th May 2024).[3] This is a comprehensive paper with useful diagrams and 277 references, but its Figure 4 includes possible pain referral patterns from lumbar facet joints, and these include 2 central symmetrical patterns along with lateralised regions. There are 3 references in the Figure legend,[4–6] and I have check all three. They are all papers that describe the pain distribution from needling and injection of lumbar facet joints and related structures. The diagrams included all illustrate lateralised pain but one paper, with no pain diagrams, does describe pain in the midline or even on the opposite side associated with needling and injection in the region of facet joints.
Personally, I think it is relatively easy to distinguish provoked pain from facet compression by using either upright (weightbearing) lumbar movements or non-weightbearing lumbar positions based on the pain severity, emotional, or (insurance etc) claim status of the individual patient.[7] The opinion of this article is that there are no reliable tests for facet pain, and I can understand that position based on the published literature.
Whilst we are on the topic of pain referral patterns, there is no mention of the typical pattern from nerve root irritation, which is a linear pattern of less than 5cm in width.[8]
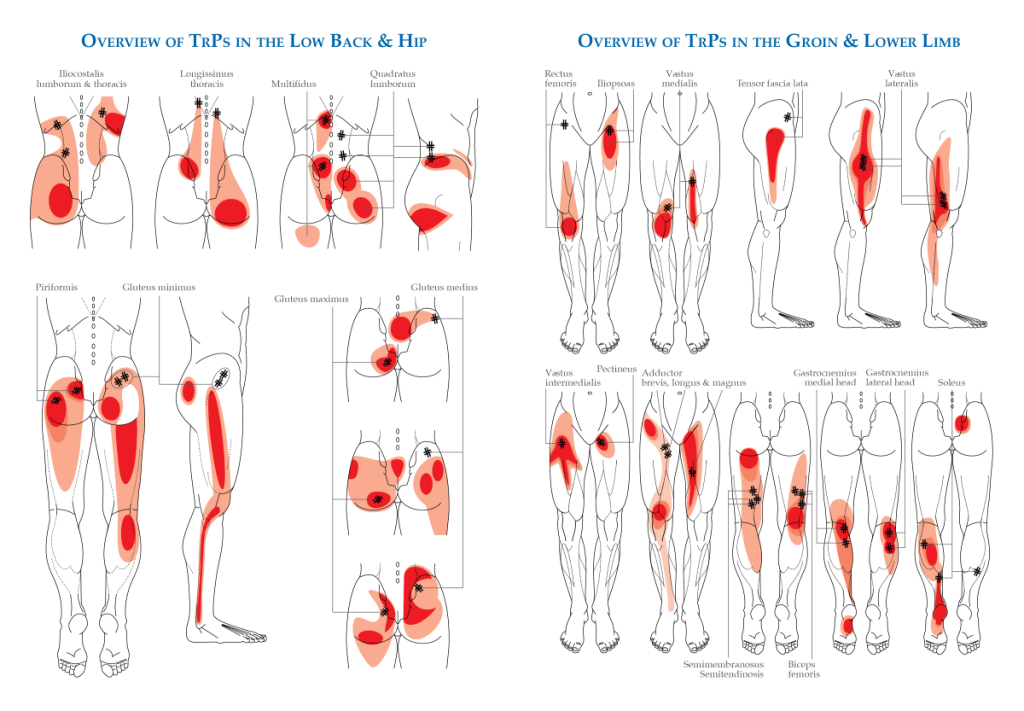
Section 3 covers myofascial pain syndrome (MPS), and it has 2 references to support the authors’ description. I confess that after checking second line references under the previous topic, and not recognising any of the names referenced in this one (a field I have been actively involved in for 3 decades), I decided not to look any further. At least MPS got a mention. The authors correctly point out that there is no diagnostic test currently available, but I imagine that they have never used a filiform needle on a TrP in clinical practice. If they had, they probably would not be asking for any diagnostic tests. Although there is not much to bill for if you have made the diagnosis and treated the patient with a needle costing 10p. Ignore me, I am bitter in my old age!
Section 4 moves to hip pathology and here they offer some useful tests, in particular tests for FAI. I don’t think I have ever diagnosed hip pathology in a patient referred with sciatica, but I have missed it in a case of posterior hip girdle pain unresponsive to needling local TrPs in gluteal muscles. So as not to fail any orthopaedic exams, I would always start with a gentle roll of the leg into internal rotation with the patient supine on an examination couch. Alternatively, for the seated patient in your consultation room you can lift the ipsilateral ankle to the side, putting the hip into internal rotation as a provocative test.
Next (section 5) is a condition that has been invented since I was at medical school (~4 decades ago). It is GTPS, previously known as trochanteric bursitis, but renamed when the bursa (under the increasingly used US imaging) refused to have enough fluid to justify the label bursitis. The test recommended is palpation of the GT… apparently it is highly sensitive and specific. We medical acupuncturists, of course, would differentiate tenderness over the GT from tenderness in the attachments of the hip abductors and TrPs in gluteus medius and minimus. This section has an interesting but rather implausible suggestion for the development of tendinopathy in the hip abductors via compression between the ITB and the GT.
Section 6 is devoted to piriformis syndrome, and has 2 references, one of which stimulated a blog here in 2019: . The subtitle of the blog was: In regret triggered by the title of Probst et al 2019.[9] I still have regret that my review paper on the topic from 2000 was not listed on PubMed.[10] It has 25% more references than the paper from 2019, and describes, for the first time, a test that has now been acknowledged (nearly 2 decades later) as the most sensitive and specific for piriformis syndrome. I’ll show you all the pictures in the Wednesday blog webinar.
Section 7 is on SIJ dysfunction, and I was pleased to see that my preferred diagnostic test was included in the short list. They call it the ‘posterior shear’ but it is also known as the 4P test – posterior pelvic pain provocation test.
Hamstring pathology fills section 8, although it seems highly unlikely that this would be mistaken for radiculopathy by any even barely competent physician IMHO.
ITB syndrome is next, and the section seems to focus only on the lateral knee pain presentation attributed to the ITB. Again, I think it would be hard to mix this up with LS radiculopathy.
Finally, we have plantar fasciitis, and the only way of mistaking this for LS radiculopathy is if you don’t actually palpate the painful area. Shocking as it might be that any clinician would not put their hands directly on the patient’s relevant part, perhaps some are distracted by the MRI images that have been produced prior to the clinical appointment.
As I sign off from this blog, as a self-styled MSK physician in the UK, my head is metaphorically well and truly in my hands.
References
1 Jorgensen SP, Chiodo AE. Musculoskeletal mimics for lumbosacral radiculopathy. Part 2: Specific disorders. Muscle Nerve. Published Online First: 5 November 2024. doi: 10.1002/mus.28279
2 Bateman EA, Fortin CD, Guo M. Musculoskeletal mimics of lumbosacral radiculopathy. Muscle Nerve. Published Online First: 10 May 2024. doi: 10.1002/mus.28106
3 Cohen SP, Raja SN. Pathogenesis, diagnosis, and treatment of lumbar zygapophysial (facet) joint pain. Anesthesiology. 2007;106:591–614. doi: 10.1097/00000542-200703000-00024
4 McCall IW, Park WM, O’Brien JP. Induced pain referral from posterior lumbar elements in normal subjects. Spine. 1979;4:441–6. doi: 10.1097/00007632-197909000-00009
5 Marks R. Distribution of pain provoked from lumbar facet joints and related structures during diagnostic spinal infiltration. Pain. 1989;39:37–40. doi: 10.1016/0304-3959(89)90173-5
6 Fukui S, Ohseto K, Shiotani M, et al. Distribution of referred pain from the lumbar zygapophyseal joints and dorsal rami. Clin J Pain. 1997;13:303–7. doi: 10.1097/00002508-199712000-00007
7 Cummings M. Low back pain assessment for the medical acupuncturist. Acupunct Med. 2004;22:189–202. doi: 10.1136/aim.22.4.189
8 Adams MA, Bogduk N, Burton K, et al. The Biomechanics of Back Pain. Edinburgh: Churchill Livingstone 2002.
9 Probst D, Stout A, Hunt D. Piriformis Syndrome: A Narrative Review of the Anatomy, Diagnosis, and Treatment. PM R. 2019;11 Suppl 1:S54–63. doi: 10.1002/pmrj.12189
10 Cummings M. Piriformis Syndrome. Acupunct Med. 2000;18:108–21. doi: 10.1136/aim.18.2.108