MSK mimics of LS radiculopathy – The BMAS Blog
Stimulated by Bateman et al 2024.[1]
MSK – musculoskeletal
LS – lumbosacral
IF – impact factor
LBP – low back pain
DRG – dorsal root ganglion
NCS – nerve conduction studies
EMG – electromyography
OA – osteoarthritis
FAI – femoroacetabular impingement
QL – quadratus lumborum
ICT – iliocostalis thoracis
RA – rectus abdominis
EDL – extensor digitorum longus
SIJ – sacroiliac joint
PFM – pelvic floor muscles– key to acronyms
This review paper popped up in my searches because it mentions myofascial pain. The topic is of particular interest because I have spent much of my clinical career assessing patients mislabelled with radiculopathy. I was intrigued to see how comprehensive this review might be, since it is published in a long-established journal with a very good reputation (IF 3.4).
The review is primarily targeted to electrodiagnostic medicine specialists, but the information is valuable for any clinician who sees LBP ie most of us.
The paper makes a good start by setting the scene with definitions of the following from Nikolai Bogduk.[2] I have edited them somewhat below, and will discuss further at the webinar.
Nociceptive back pain – pain that is evoked by noxious stimulation of structures in the lumbar spine
Somatic referred pain – pain referred from somatic structures (in this case from noxious stimulation of structures in the lumbar region) to the hip girdle and lower limb
Radicular pain – pain derived from direct irritation of nerve roots (usually chemical irritation from the inflammation around extruded disc material)
Radiculopathy – a neurological state (not defined by pain) in which nerve conduction is blocked along a nerve root (usually as a result of compression)
I love reading Bogduk – he is so clear, precise, and logical. He is apparently a fearsome character, but I would love to meet him and discuss the few areas where our positions diverge ever so slightly. One of the latter comes from his assertion that radicular pain derives physiologically from ectopic discharges emanating from a dorsal root or its ganglion. My position is that the pain is more likely to derive from sensitised nerve endings in the nerve root sheath. Ectopic activity in nerves occurs as a result of damage to axons. The majority of patients with radicular pain have no indication of nerve damage.
Back to the review and the first figure is a dermatome map of the lower limb. Normally I worry about the appearance of such a map when discussing pain conditions, since most MSK pain does not come from the skin. In this case it is useful and relevant because radiculopathy can manifest as numbness within the relevant dermatome, despite being relatively uncommon in LBP as a whole.
The authors go on to list the sensory and motor signs relevant to each level from L1 to S4. This then leads to a list of possible MSK mimics of radiculopathy at each level. It is a comprehensive list and even includes a couple of diagnostic labels that I do not draw from in my practice. Both have been developed from increased use and sophistication of imaging rather than specific clinical examination findings – ischiofemoral impingement and gemellus / obturator internus syndrome.
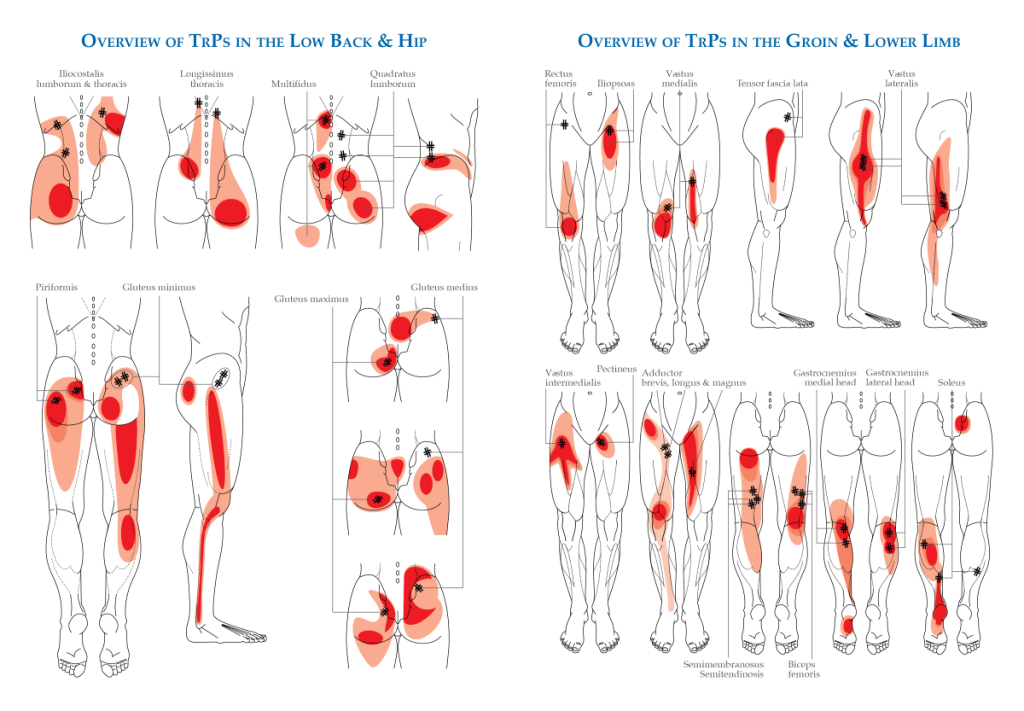
Myofascial pain gets mentioned, but not in detail, and unfortunately, we don’t have the likely muscles listed for each segmental level. I will attempt to add them to the author’s list of MSK mimics below. In one series, myofascial pain made up nearly 40% of referrals for electrodiagnostic testing (motor and sensory NCS and EMG) in suspected lumbosacral radiculopathy, where the NCS turned out to be normal.[3] Myofascial pain made up 12% of the group who had positive NCS.
L1
Hip OA
Femoral head avascular necrosis
Labral tears and/or FAI
Athletic pubalgia (used to be called osteitis pubis)
Possible TrP sources: QL / ICT / L1 multifidus / RA / external oblique / adductor magnus
L2
Occult femoral neck fracture or stress fracture
Iliopsoas bursitis or tendinopathy
Possible TrP sources: iliopsoas / pectineus / adductors
L3
Greater trochanteric pain syndrome
Iliotibial band syndrome
External snapping hip syndrome
Possible TrP sources: TFL / glutes / vastus lateralis
L4
Quadriceps muscle injury
Knee OA
Possible TrP sources: rectus femoris / quads / sartorius / adductors
L5
Piriformis syndrome
Exertional compartment syndrome
Tibial and/or fibular stress syndrome
Possible TrP sources: piriformis / gluteus minimus / L5 multifidus / fibularis / EDL
S1
Hamstring strain or tendinopathy
Ischiofemoral impingement
Ischiogluteal bursitis
SIJ dysfunction
Plantar fasciitis
Possible TrP sources: piriformis / hamstrings / gastrocs / soleus
S2-4
Gemellus / obturator internus syndrome
Coccydynia
Possible TrP sources: gluteus maximus / sacral multifidus / adductor magnus / PFM
At any level there could be referral from spinal structures such as facet joints in the absence of radiculopathy.[4] The role of interspinous ligaments is mentioned, but this is rather controversial, and I will say more about that on Wednesday evening.
Before finishing, I should note my favourite textbooks on back pain,[5,6] which have help me tremendously in developing an understanding of this almost inevitable human condition.
References
1 Bateman EA, Fortin CD, Guo M. Musculoskeletal mimics of lumbosacral radiculopathy. Muscle Nerve. Published Online First: 10 May 2024. doi: 10.1002/mus.28106
2 Bogduk N. On the definitions and physiology of back pain, referred pain, and radicular pain. Pain. 2009;147:17–9.
3 Cannon DE, Dillingham TR, Miao H, et al. Musculoskeletal disorders in referrals for suspected lumbosacral radiculopathy. Am J Phys Med Rehabil. 2007;86:957–61.
4 Cohen SP, Raja SN. Pathogenesis, diagnosis, and treatment of lumbar zygapophysial (facet) joint pain. Anesthesiology. 2007;106:591–614.
5 Bogduk N. Clinical anatomy of the lumbar spine and sacrum. Edinburgh: Chirchill Livindstone 1997.
6 Adams MA, Bogduk N, Burton K, et al. The Biomechanics of Back Pain. Edinburgh: Churchill Livingstone 2002.
Published




