PID resorption 2024 – The BMAS Blog

Stimulated by Albert et al 2023.[1]
PID – prolapsed intervertebral disc
LBP – low back pain
NSAIDs – non-steroidal anti-inflammatory drugs
SD – standard deviationkey to acronyms
This paper was published online in mid-December but I could not access the full text. I wrote to the first author, Hanne Albert, and she kindly sent me the pdf along with a couple of other papers on a related theme. I recognised her name from a rather interesting study some 10 years ago that demonstrated the effect of a course of antibiotics on chronic LBP in a specific subgroup of patients.[2]
This is another paper that seemed to come out of nowhere with potentially major implications for how LBP with lumbar PID is managed.
It is not a controlled trial, but a prospective cohort study using MRI every 3 months to assess disc resorption in patients with acute PID and leg pain. That alone is quite interesting because it gives us useful information for advising patients on how long their sciatica might take to resolve. The really novel aspect to this study is that they specifically avoided the use of NSAIDs or steroids (including steroid injections), but instead they prescribed gabapentin and provided 12 sessions of acupuncture every 3 months.
Sagittal MRI images were used to measure the size of the extruded disc material and ‘complete resorption’ was defined as a reduction in size of 40% or more along with a reduction in leg pain of 70% or more.
90 patients were assessed – just over half were female and the average age was just under 49. The mean PID size at initial assessment was 120mm2, with an SD of just over 50mm2. 19 patients achieved complete resorption by 3 months, a further 44 by 6 months, and then 21 and 6 in the last 2 quarters of the study. The average time to complete disc resorption was 4.4 months and by 12 months 100% of patients had achieved complete disc resorption.
Initial size of the PID did not correlate with the rate of resorption in this study, but size is likely to be important and it may be that the study was not large enough to demonstrate this relationship. Leg pain and dose of gabapentin at baseline was weakly correlated with the initial size of the PID.
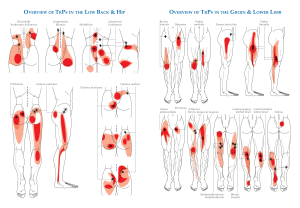
Acupuncture was applied once a week and involved the use of 10 to 20 needles with a retention time of 20 minutes. From the data in one of the tables in the paper it looks as though almost all patients had all the available sessions of acupuncture in the first 2 periods (6 months), but very few continued to have acupuncture after this.
Some readers may wonder about the anti-inflammatory effects of acupuncture, which have figured prominently on this blog and seem to run slightly counter to the principle of this study. Well, the acupuncture, or more correctly, the EA data demonstrate systemic anti-inflammatory effects rather than localised effects. Indeed, my experience is that localised acute inflammation, such as acute rheumatoid arthritis, is not influenced to any degree by acupuncture in the clinical setting, while some effects can be measured in laboratory studies.
If you want to try this protocol without the use of gabapentin, I suggest EA twice or 3 times a week initially to optimally control the pain.
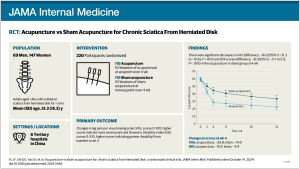
Clearly further research is needed, since this is an uncontrolled trial, but I would be keen to see a pragmatic controlled trial next, with conventional treatment using NSAIDs and steroid injection compared with this inflammation preserving approach. It seems likely that the latter, as tested here, will result in more rapid resolution of symptoms, since 4.4 months is considerably better than the 8 to 9 months that we are familiar with.
Finally, I have mentioned regression of lumbar PIDs previously on this blog (see: ). The observations in this previous blog do seem to be consistent with the current one, in that active inflammation around the extruded disc seems to be associated with more rapid regression.
References
1 Albert HB, Sayari AJ, Barajas JN, et al. The impact of novel inflammation-preserving treatment towards lumbar disc herniation resorption in symptomatic patients: a prospective, multi-imaging and clinical outcomes study. Eur Spine J. Published Online First: 15 December 2023. doi: 10.1007/s00586-023-08064-x
2 Albert HB, Sorensen JS, Christensen BS, et al. Antibiotic treatment in patients with chronic low back pain and vertebral bone edema (Modic type 1 changes): a double-blind randomized clinical controlled trial of efficacy. Eur Spine J. 2013;22:697–707.
Published